Recurrent Implantation Failure: What Is It and When Does It Really Exist?
One of the most common reasons patients come to me is the “recurrent implantation failure.” Patients often say things like:
“I’ve tried everything. Nothing works. What’s wrong with me? What am I doing wrong? My uterus just won’t implant them…”
The first thing we need to remember is that humans, as a species, are not very fertile. If we took 100 couples, each 25 years old, and asked them to have unprotected sex for one month, only about 25 to 30 would get a positive pregnancy test. Why? There are many reasons, but a large part is because we often produce abnormal gametes—eggs and sperm—far more frequently than most other species.
If we tried this same experiment in dogs, rabbits, or mice, the numbers would be very different: between 60% and 95% success, depending on the species. But we are simply not that efficient. Which means we often have to try more than once.

The Importance of Patience and Persistence
This helps explain why trying for 6 to 12 months (depending on age) is recommended before seeking fertility care—and why patience and persistence are essential words in fertility treatment.
Live birth rates per embryo transfer are roughly:
-
40-45% at age 30
-
35% at age 35
-
20% at age 40
So, a 35% chance of success per attempt is not a bad chance—but it does mean that 1 out of 3 attempts may succeed… and 2 out of 3 may not.
To picture this: imagine a lottery drum with three balls—one says “YES,” and the other two say “NO.” You’re more likely to pull a “NO” on each individual attempt. But if you keep trying, eventually you’ll draw the winning ball.
That’s key: failure is more likely per attempt, but success is more likely per person or couple because most people eventually do achieve pregnancy.
Is It Really Recurrent Implantation Failure?
The term “recurrent implantation failure” (RIF) can feel like a heavy label. That’s why we should use it cautiously. It’s not accurate to talk about RIF after just 2 or 3 failed embryo transfers. Doing so may lead to:
-
Switching strategies too soon
-
Unnecessary costs and stress
-
Added frustration
-
Adopting the mindset of “I’m one of the ones who can’t” when that may not be true
Most failed transfers are due to embryo-related issues, not problems with the uterus or immune system. Even in cycles with tested euploid embryos (via PGT-A), implantation rates rarely exceed 60–70%. This means many failures happen for no clear or fixable reason.
What If I’ve Already Tried Elsewhere?
Not all clinics, labs, or doctors have the same success rates. While many may offer “IVF” or “egg donation,” not all programs are equal.
In countries like the U.S., where clinic-specific success rates are published, we clearly see wide differences in outcomes. So, if a treatment didn’t work in one clinic, that doesn’t mean it won’t work elsewhere.
For example, an egg donation program with a 60% success rate is not comparable to one with 30%. It’s not always about doing something different—sometimes it’s about doing the same thing better.
What If It Is a True Case of RIF?
If multiple treatments have failed under optimal conditions (good clinic, lab, physician, and embryologist), it’s worth taking a closer look.
But personalized medicine does not mean trying anything just because it “might work” in your case. It means adapting treatment based on the best available evidence.
Now is not the time for guesswork. Shotgun approaches are rarely a good strategy.
What Tests Could Be Considered?
Some strategies worth exploring (with varying degrees of evidence):
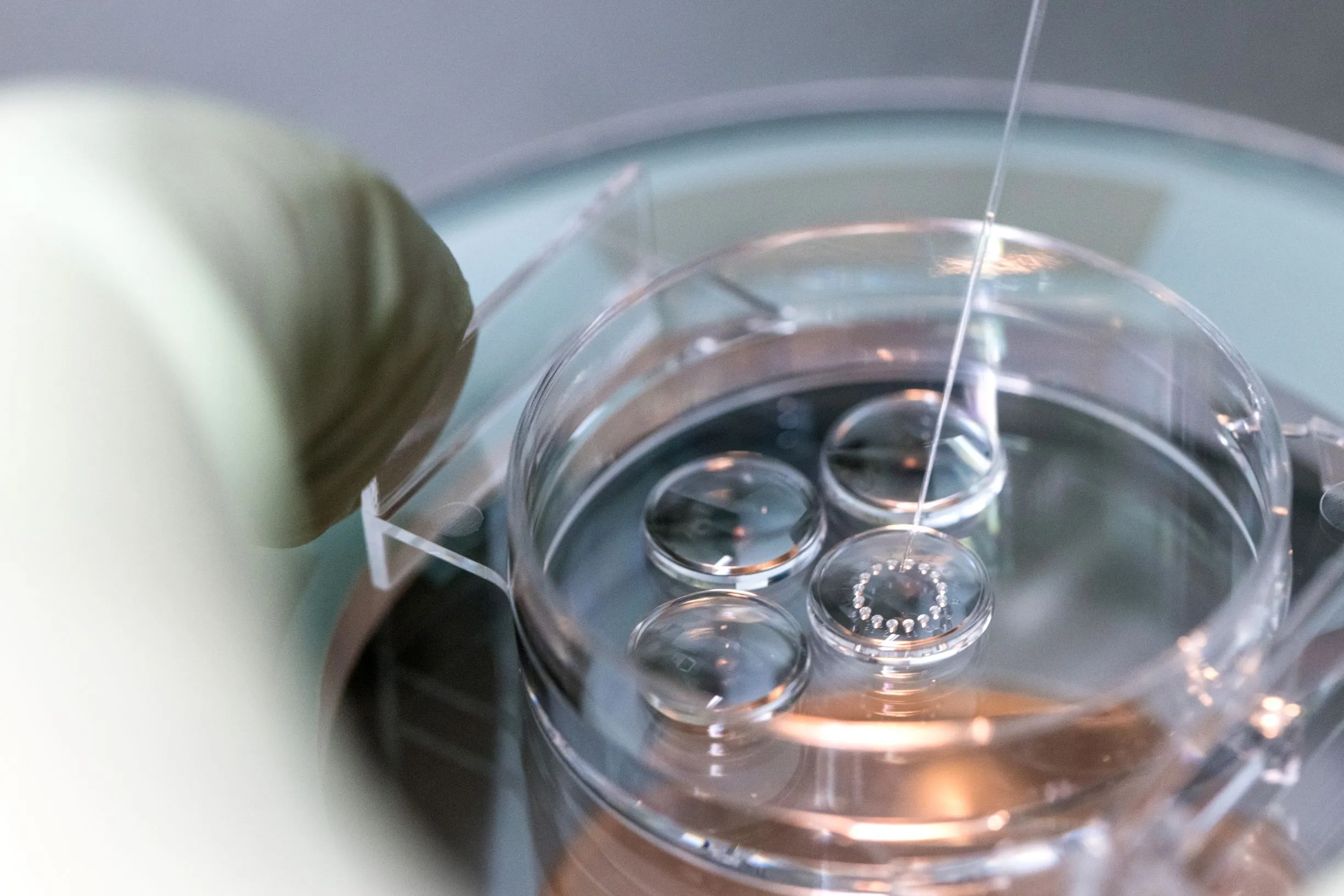
🔬 Embryo testing (PGT-A)
To reduce the chance of transferring abnormal embryos.
🧫 Endometrial assessment
-
Hysteroscopy
-
Biopsy to rule out chronic inflammation or endometritis
-
Endometrial receptivity testing (e.g. ERA) → usefulness still debated
🧬 Uterine microbiome analysis
May provide insight in selected cases, though the evidence is still limited.
🧪 Use of donor gametes
Especially egg donation, if subtle egg quality issues are suspected.
🚫 Thrombophilia screening, natural killer cells, immunology panels, endometrial scratching
These approaches haven’t shown benefit in well-conducted studies and are not generally recommended in most international guidelines.
In Summary
-
Most patients worried about implantation failure do not have true RIF.
-
It’s more likely they fall within normal success rates, which often require several attempts.
-
If treatment isn’t working, consult a fertility expert who can evaluate your case with objectivity and evidence.
-
Success doesn’t always come from doing something different, but rather from doing it well, with the right team, in the right setting.
Take-home message
In reproductive medicine, small details can make a big difference. Our approach is grounded in science, experience, and truly listening. A careful and objective evaluation of each case can not only clarify what’s happening but also guide decisions that may improve the chances of success. If you feel like you’ve reached a standstill, it might be worth looking at things from a fresh perspective.